Flesh-Eating Bacteria at the Beach? What You Need to Know.
Infections with Vibrio vulnificus are rare, especially in the Northeast. But a few recent cases suggest that precautions are wise for some wading into the water.
The News
With Labor Day and the start of a new school year looming, throngs of New Yorkers will head to the beach this weekend, braving traffic, sunburns, maybe sharks — and Vibrio vulnificus, a nasty, flesh-eating bacteria that thrives in warm seas and brackish water.
Since the beginning of July, four people in the greater New York area have been infected with the bacteria, including three who have died, according to health officials in New York and Connecticut.
Two of the people sickened in Connecticut had been exposed to saltwater or brackish water in the Long Island Sound. One had eaten raw oysters, which can become infected with the bacteria during warm spells. (The cause of the fourth infection, which killed a Suffolk County resident, is not known.)
“If we were having this conversation 15 years ago, we’d be talking about infections along the Gulf Coast,” said Dr. William Schaffner, an infectious disease specialist at Vanderbilt University School of Medicine. “But now these infections are creeping up the East Coast.”
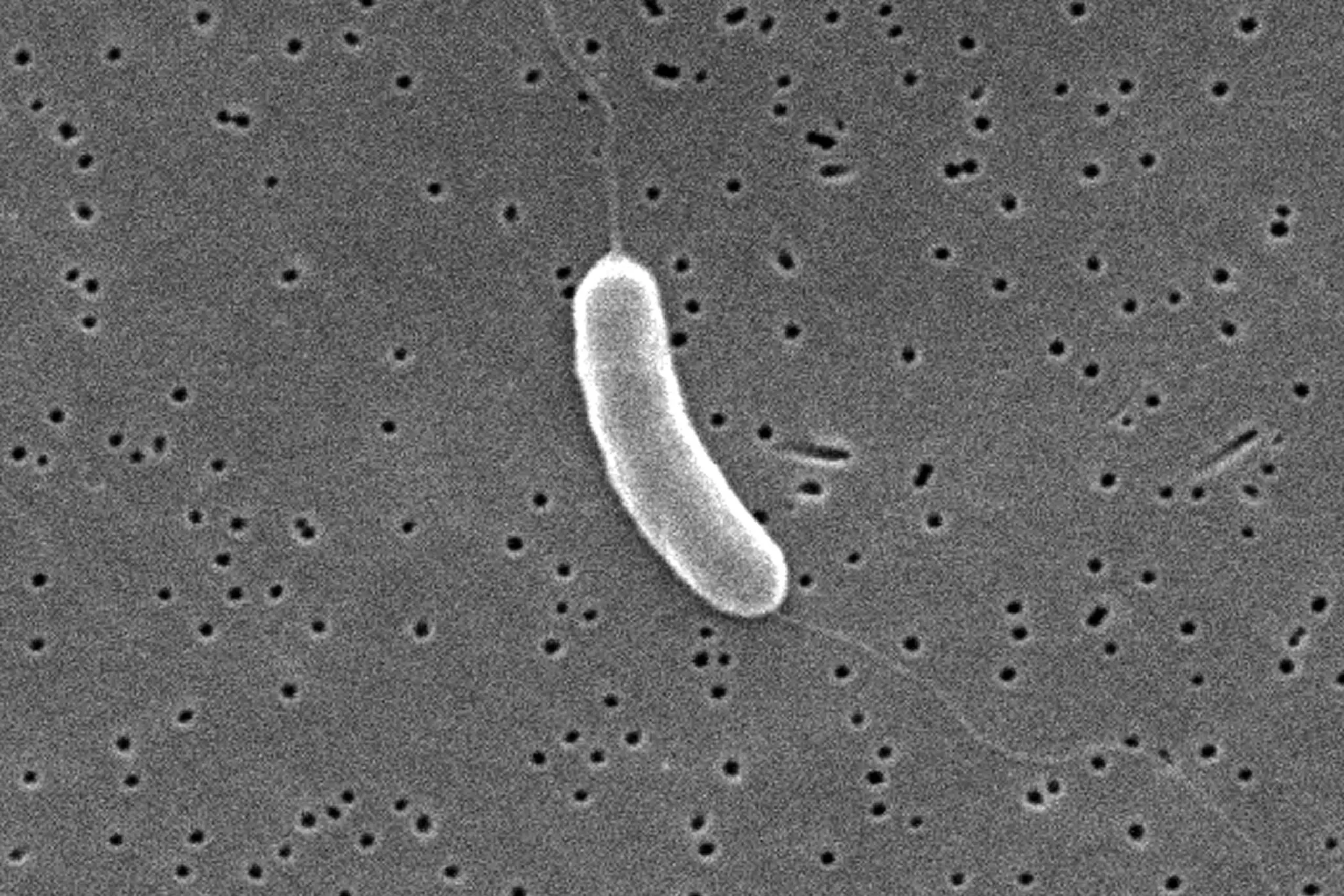
The bacteria Vibrio vulnificus is related to the type that causes cholera.Credit…Janice Haney Carr/Centers for Disease Control and Prevention
The Back Story: An infection that surprises beachgoers.
It’s not clear whether the appearance of these cases farther north than usual may be a result of better diagnosis or to warming waters associated with climate change.
The illness, technically called vibriosis, may be caused by infection with several related bacteria. Among the worst is V. vulnificus, which is relatively rare but can be deadly for those who are vulnerable, with mortality rates as high as 33 percent, according to one scientific paper.
The bacterium spreads most commonly in two ways.
When people swim in waters contaminated with V. vulnificus, an open sore or cut can provide an entry point for the organism. From there it spreads, becoming a so-called flesh-eating infection that extends quickly beyond the wound into healthy tissue. Then it may spill over into the bloodstream, causing a life-threatening condition called sepsis.
The bacterium also spreads when people who are immunocompromised or have liver disease eat raw oysters that are contaminated. Physicians warn patients with these conditions against eating raw oysters, which become infected by seawater they filter for food.
Older people are generally at greater risk. The three patients who fell ill in Connecticut were all over age 60. People who take medications to reduce stomach acid may also be more likely to get infected or to develop complications following infection.
If you’re among the vulnerable, wear shoes that protect against cuts and scrapes when you’re in salty or brackish water. Wear protective gloves when handling raw seafood. Avoid swimming in the ocean if you have a cut, scrape or other abrasion that might let in the bacterium.

What to Watch: The bacterium seizes on openings.
Vibriosis causes a wide range of symptoms, including diarrhea and stomach cramps, vomiting, fever, chills, ear infections and wound infections.
The intestinal problems occur more quickly in people who have ingested the bacterium, usually by eating raw oysters. Ear and wound infections will become red, swollen and extremely painful over a bit more time. Blisters filled with clear liquid may appear on the skin.
Symptoms usually appear within 12 to 24 hours of exposure, and people should seek medical care as soon as possible. Tell doctors about the exposure: The infection can spread quickly if left untreated.
“If the wound starts to look red, puffy and painful, or has a discharge, or redness spreading beyond the edges of the wound, you need to get medical attention right away,” Dr. Schaffner said. “Don’t try to tough it out and wait to see if it gets worse tomorrow.”
A lab test is needed to make the diagnosis. Treatment involves antibiotics and supportive care, but surgery may be required to clean out an infected wound and stop the spread of the infection.
Your Beach Weekend: The vulnerable should exercise caution.
Consider avoiding the water, and not even walking on the beach or wading, if you have an open wound, including one from a recent surgical operation or piercing or tattoo. An open wound means any cut, scrape or other abrasion that might allow the bacterium into your body.
If there is a chance your wound could come into contact with saltwater or brackish water, marine life, or raw or undercooked seafood while you’re cooking, swimming, fishing, boating or walking on the beach, cover the open wound with a waterproof bandage.
If a wound or cut does comes into contact with brackish water or saltwater, raw seafood or its juices, wash it thoroughly with soap and water. If you develop a skin infection, let your health provider know quickly — this is an infection that can spread rapidly.
What’s Next: Watch for the infection in unexpected places.
Climate change will test all of us in unexpected ways. Vibrio infection is something Americans living in the Northeast may need to watch for now.
If you have cancer, are immunocompromised, have liver disease or take drugs to lower stomach acid, doctors say you should not eat raw or undercooked oysters or other raw or undercooked shellfish. (Of course, the same is true for pregnant women.)
If you’re handling raw shellfish, wash your hands thoroughly with soap and water afterward.
An earlier version of this article incorrectly described rate at which people die of V. vulnificus infection. Thirty-three percent is the mortality rate, not the survival rate.

San Jose woman loses limbs after battling bacterial infection from tilapia
There’s a warning about a dangerous bacteria that might have infected a local woman who’s still recovering after nearly two months in the hospital. An online fundraising effort says she contracted the bacterial infection after eating fish and is now a quadruple amputee.
The Centers for Disease Control and Prevention (CDC) recently issued a warning about a bacterial infection that people can get by eating raw or undercooked fish or by exposing an open wound to coastal waters. A friend tells us this San Jose woman likely got this specific infection after eating undercooked tilapia.
A San Jose mother’s life is changed forever. Laura Barajas, 40, has had her limbs amputated while battling a bacterial infection.
“It’s just been really heavy on all of us. It’s terrible. This could’ve happened to any of us,” said Barajas’ friend Anna Messina.

Messina says back in late July Barajas had bought tilapia from a local market for dinner. She cooked it and ate it alone. Within days, she got very ill and was then hospitalized.
“She almost lost her life. She was on a respirator,” Messina said. “They put her into a medically induced coma. Her fingers were black, her feet were black her bottom lip was black. She had complete sepsis and her kidneys were failing.”
Now, a month and a half later, Barajas is without her arms and legs.
Messina believes the infection was caused by Vibrio vulnificus — a bacterial infection the CDC has been warning about.
“The ways you can get infected with this bacteria are one-you can eat something that’s contaminated with it the other way is by having a cut or tattoo exposed to water in which this bug lives,” said UCSF Infectious Disease Expert Dr. Natasha Spottiswoode.
Spottiswoode says the bacteria is especially concerning for people who are immunocompromised.
The CDC says about 150-200 cases of the infections are reported each year and about one in five people with the infection die — sometimes within one to two days of becoming ill.

“People should take sensible precautions like if you have a cut avoid getting immersed in water until it’s well healed,” Spottiswoode said. “If you are someone immunocompromised keeping an eye on these things and avoiding those high-risk activities and foods.”
Messina says she and Barajas’ family are still waiting to learn more about what happened. She hopes people realize how precious life can be.
“Be thankful for what we have right now because it can be taken away so quickly so easily,” Messina said.

Messina set up a GoFundMe to help with her friend’s medical expenses. So far, it has raised more than $95,000.
Sepsis Can Cause a Red Line on Your Skin—Here’s What You Need To Know
Noticing this mark on your skin can be a warning sign.
At least 1.7 million adults in America develop sepsis each year. And at least 350,000 adults who develop sepsis die during their hospitalization or are discharged to hospice each year.1
Sepsis is one of the oldest described illnesses (first described back in 400 BCE), and it’s also been on the rise since 2000.2 Learn about this potentially fatal condition, how to recognize symptoms—one being a red line on your skin—and when to seek treatment.

FACEBOOK.COM/ ALEXANDRA RUDDY
What Is Sepsis?
Sepsis is a potentially life-threatening condition caused by an extreme reaction the body has to infection. It happens when an infection you already have triggers a chain reaction throughout your body.1
When sepsis occurs, it can progress rapidly. In severe cases, one or more organ systems fail. In the worst cases, blood pressure drops, the heart weakens, and the patient spirals toward septic shock. Once this happens, multiple organs—lungs, kidneys, liver—may quickly fail, which is usually fatal.3
“Sepsis is the most serious form of any infection,” Frank Esper, MD, pediatric infectious disease specialist at Cleveland Clinic, told Health. “Sepsis is when you have an infection so bad it is disseminating across the body—kidneys shutting down, liver shutting down, heart’s in trouble.” Seeking medical care quickly is of the utmost importance once you see symptoms, which may include mental decline, a fever, and fatigue.
Sepsis Symptoms and Diagnosis
Common symptoms of sepsis are fever, chills, rapid breathing and heart rate, rash, confusion, and disorientation. Many of these symptoms are also common in other conditions, making sepsis challenging to recognize, especially in its early stages.3 If you have the following symptoms, your healthcare provider may diagnose sepsis:4
- Fever
- Low blood pressure
- Increased heart rate
- Difficulty breathing
Healthcare providers may also perform tests to check for signs of infection or organ damage or to identify the bacteria that caused the infection that led to sepsis.4
They may also perform a chest X-ray or a CT scan to locate an infection. In addition, they can use a scoring system to determine if the function of a particular organ is declining and note the number of organ systems affected.3
A Red Mark or Red Line
One of the symptoms of sepsis is a rash that does not fade when you press it.5A red mark may appear if an infection travels through the lymph nodes to other body parts. “It’s very concerning. You need to be on antibiotics immediately,” said Dr. Esper, adding that his team sees these marks often.
Red streaks or a red line on the skin may be a sign of lymphangitis. Lymphangitis is an infection of the lymph vessels and is a complication of some bacterial infections such as streptococcal infection or staphylococcal infection. The infection causes the lymph vessels to become inflamed.6
Lymphangitis may be a sign that the bacteria is spreading into the blood and may develop into sepsis, which can cause life-threatening problems. The red streaks can spread within a few hours. Fever, chills, and malaise may accompany lymphangitis.7
Dr. Esper said there’s a simple way to track whether redness around a wound is spreading, which could signal infection. “Take a pen and mark around the site. Draw a border around the redness. Does the redness go beyond that mark [the next day]? If you’re on antibiotics and the redness goes beyond those markings, we’re on the wrong antibiotics, or we need something more powerful.”
Causes of Sepsis
Sepsis is caused by infections. Bacterial infections cause most cases of sepsis. But sepsis can be caused by viral or fungal infections, too.
Normally, the body releases chemicals into the blood to fight infection. If unchecked, these chemicals trigger widespread inflammation, blood clots, and leaky blood vessels. As a result, blood flow is impaired, depriving organs of nutrients and oxygen and leading to organ damage.3
Risk Factors
Anyone can get an infection that could potentially lead to sepsis. But some people are at greater risk for the urgent conditions. They include:1
- Adults 65 or older
- People with weakened immune systems
- People with chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease
- People with recent severe illness or hospitalization
- People who survived sepsis
- Children younger than one
Treatment
Healthcare providers should treat sepsis with antibiotics as soon as possible. Antibiotics are critical tools for treating life-threatening infections, like those that can lead to sepsis.
Fast detection and initial treatment of sepsis are of utmost importance. Research shows that rapid, effective sepsis treatment includes:4
- Giving appropriate treatment, including antibiotics
- Maintaining blood flow to organs
- Getting surgery to remove tissue damaged by the infection
Individual immune responses and responses to treatment such as antibiotics may vary. Scientists are continually trying to find new therapies and determine which individuals are likely to benefit most from certain approaches.3
A Quick Review
Sepsis is the most serious form of infection, yet anyone can develop the potentially fatal condition. Sepsis is the body’s extreme response to an infection. It is life-threatening, and without timely treatment, sepsis can rapidly lead to tissue damage, organ failure, and death.
Being educated about the symptoms of sepsis and seeking out medical treatment are critical to successful recovery from sepsis